A health savings account is a tax-advantaged savings account that can be funded by individuals whose only health care coverage is a qualified high deductible health plan . An HSA is an alternative way for you to pay for your qualified health care expenses and save for future qualified health care expenses on a tax-free basis. Expenses such as out-of-pocket costs for office visits, prescription drugs, dental expenses and laboratory tests may be paid for from your HSA. Once funds are deposited into your HSA, those funds can be used to pay for qualified medical expenses tax-free, even if you no longer have high-deductible health plan coverage.

The funds in your account automatically roll over each year and remain in the account indefinitely until used. Once you discontinue coverage under a high-deductible health plan and/or get coverage under another health plan that disqualifies you from an HSA, you can no longer make contributions to your HSA. However, since you own the HSA, you can continue to use it for future qualified medical expenses. Under the last-month rule, if you are an eligible individual on the first day of the last month of your tax year , you are considered an eligible individual for the entire year.

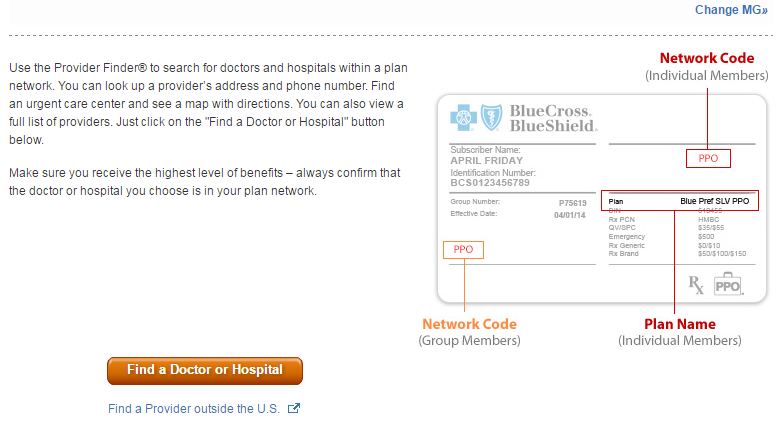
What Is The Group Number On Your Insurance Card You are treated as having the same high-deductible health plan coverage for the entire year as you had on the first day of that last month. The total contribution for the year can be made in one or more payments at any time up to your tax-filing deadline . However, if you wish to have a contribution made between January 1 and April 15 treated as a contribution for the preceding tax year, please contact the HSA bank. You cannot use HSA funds to pay for qualified medical expenses incurred before you enrolled in a high-deductible health plan. In order to establish an HSA, you must enroll in a high-deductible health plan.

Your eligibility to contribute to an HSA is determined by the effective date of your high-deductible health plan coverage. To enroll in a high-deductible health plan, complete the Blue KC application process. The Blue-Saver® PPO health insurance plan is a high-deductible health plan that allows you to establish an HSA as part of your health benefits.

When you enroll in the Blue Saver plan, you may be offered the opportunity to establish a HSA with one of our preferred banks. You will be presented with appropriate banking authorizations and disclosures necessary for Blue KC to work with the bank that will establish your HSA. Please note all financial institutions offering HSA products must comply with the USA Patriot Act, requiring your HSA bank to collect and verify information about you when processing your HSA application. Once your HSA has been established, you will be mailed a welcome kit and HSA debit card from the bank. A Health Savings Account allows members enrolled in a qualified high-deductible health plan to contribute funds on a tax-free basis into the member's account. A member's employer may also contribute funds to the account.
These funds are used for payment of qualified medical expenses as defined by the IRS. Unused funds in an HSA roll over in the member's account at the end of each calendar year. If you're an HMO member, you will need to receive services from an in-network HMO provider. However, you will be able to receive emergency or urgent care services no matter where you are. For details about your coverage, please review your Blue KC certificate, which outlines the benefits and exclusions related to your health insurance plan.

You can view your certificate by logging in and accessing the Plan Benefit section. This federal mandate applies to all individual policies, fully insured group health plans and both ERISA and non-ERISA self-funded groups, where the state law does not apply. An Exclusive Provider Organization is designed for integration of a healthcare plan, health providers and an insurance company. An EPO plan manages cost by improving quality and health of members by using select providers . An EPO plan promotes quality through transparency initiatives and policies that promote member health and manage the care members receive. An EPO plan often covers services in-network with network providers and has $0 benefits for out-of-network.
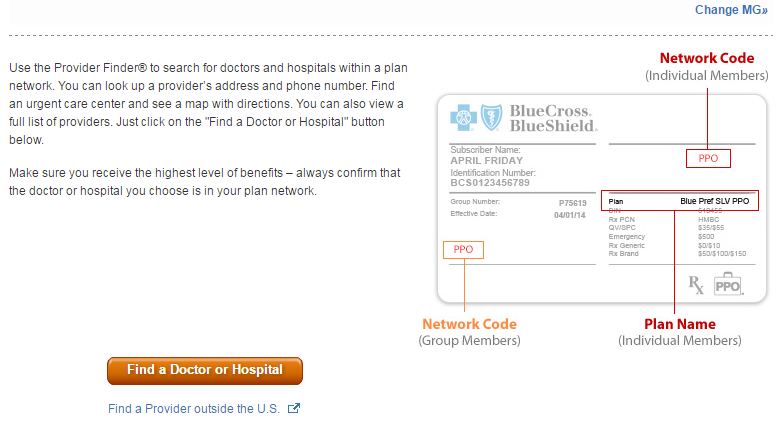
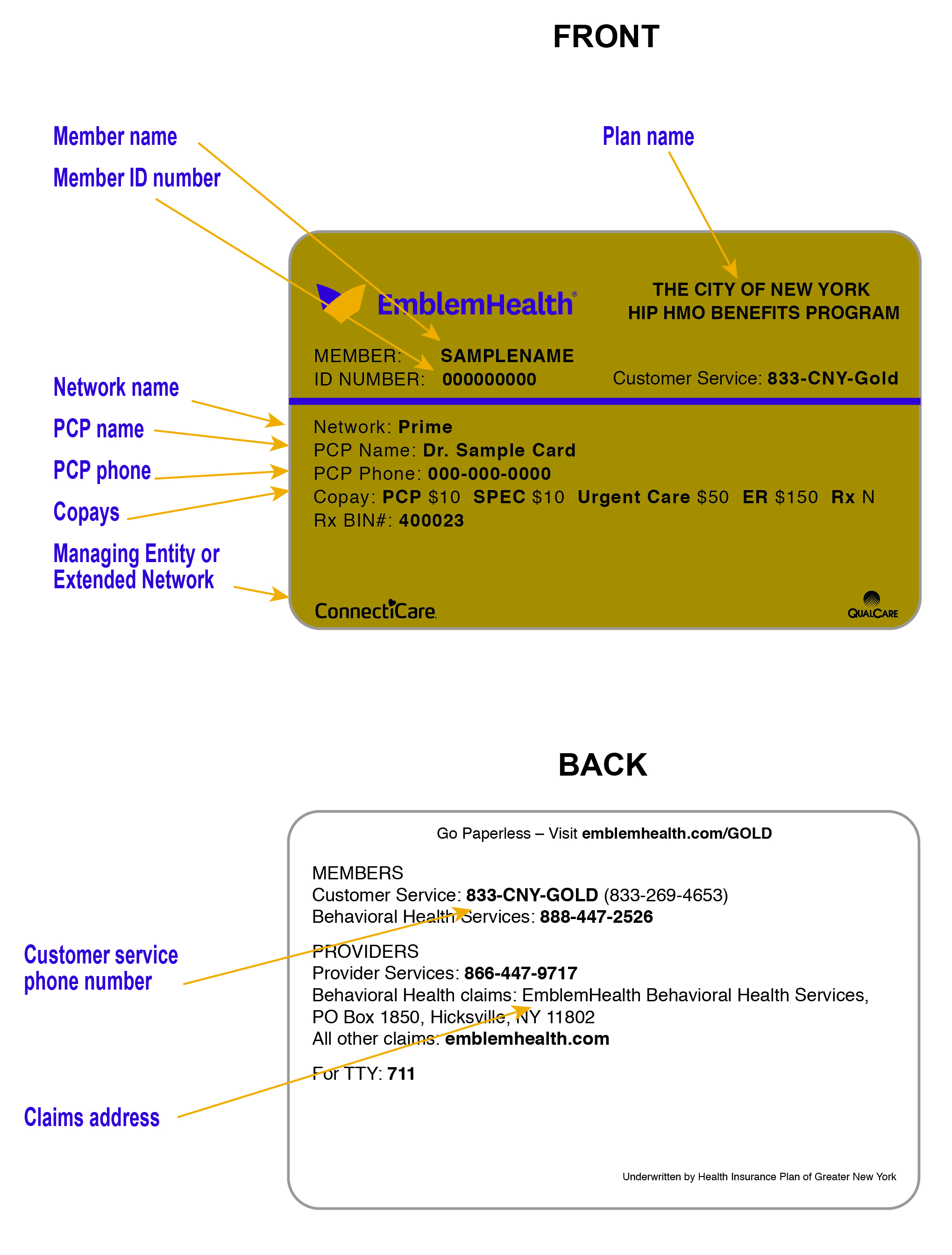
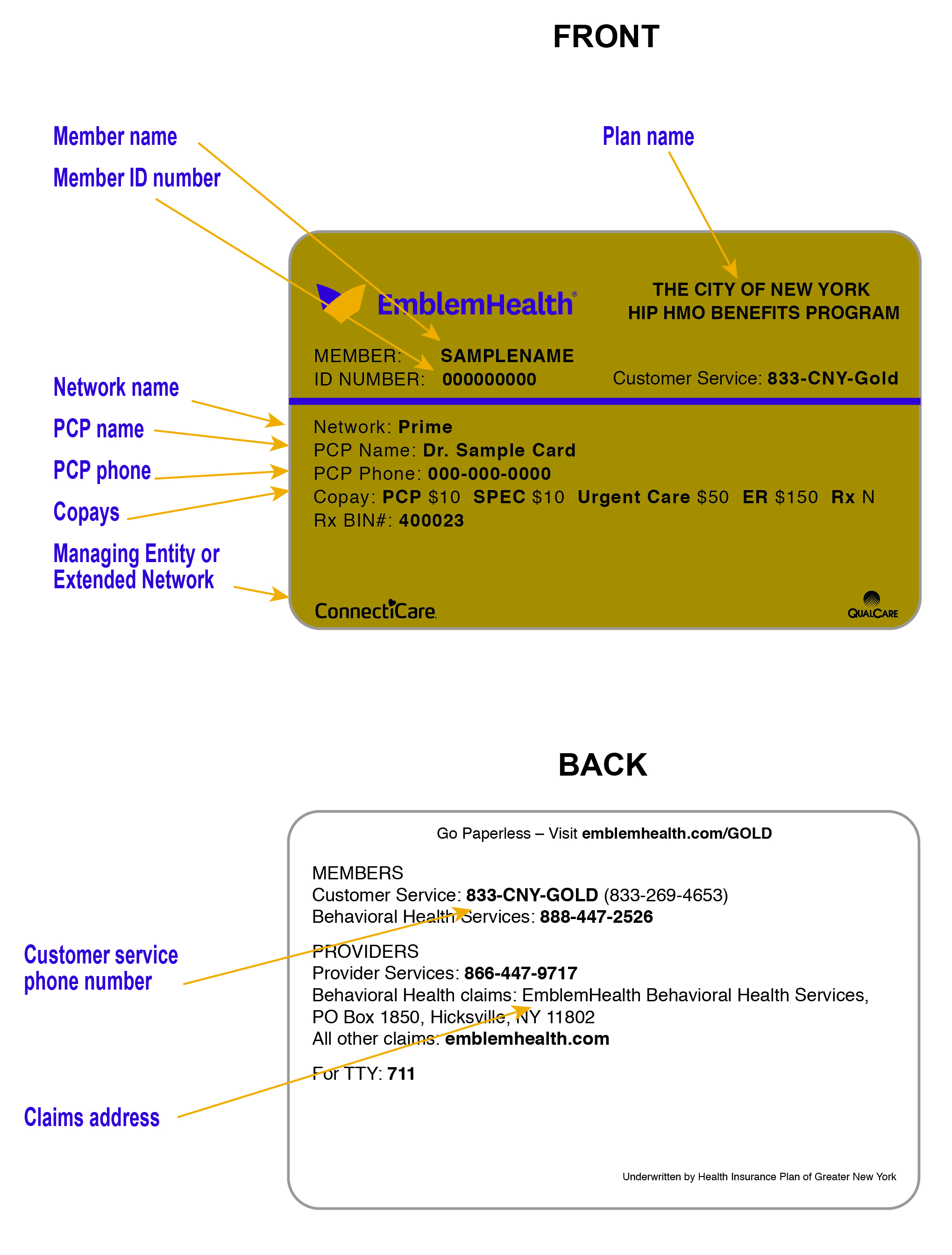
The maximum amount that may be contributed to your HSA for any year is a certain amount established annually by the IRS. This amount depends on whether you have individual or family coverage under your qualified high-deductible health plan. The same annual contribution limit applies regardless of whether the contributions are made by an employee, an employer or both. To change a PCP, log in and visit you Profile by clicking on the icon by your name in the top right corner of your homepage. In the Coverage Information section you'll see a list of covered members for your Blue KC policy.

From here select "Change PCP" for the appropriate member and you can search for and designate a new PCP. Once we have processed your PCP change request, we will send you a new member ID card that contains the information of your newly selected PCP. You may also call the Customer Service number listed on your member ID card to change your PCP. Please note that if you have health insurance through your employer, you may be required to contact your group benefits administrator to change your PCP. Coordination of benefits is the process used when a member has two health insurance plans. This process allows the two plans to work together getting you the most out of your coverage.

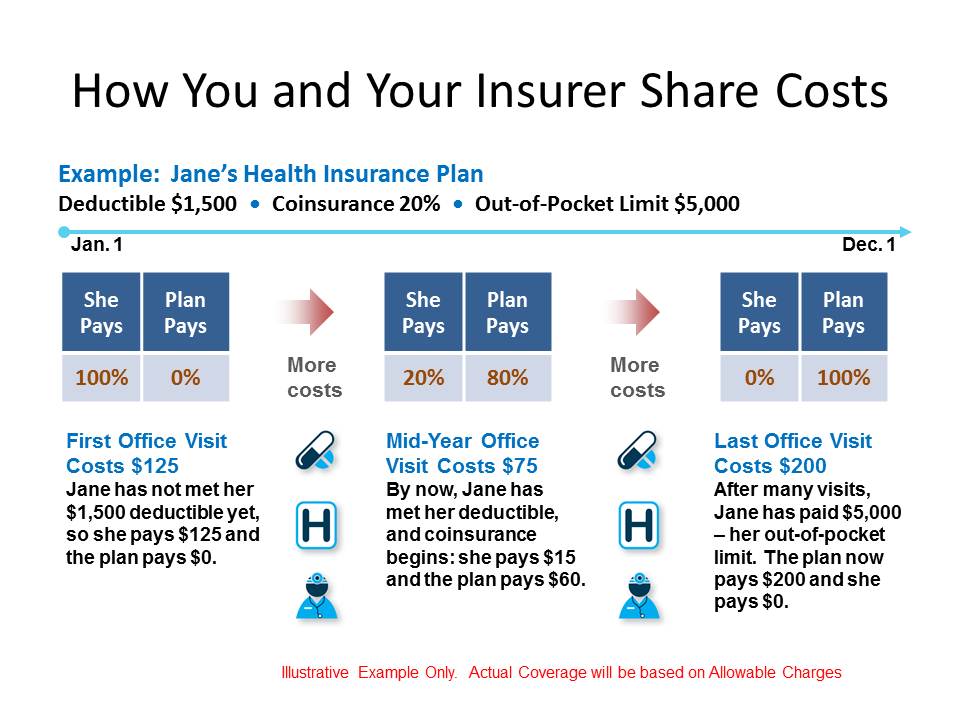
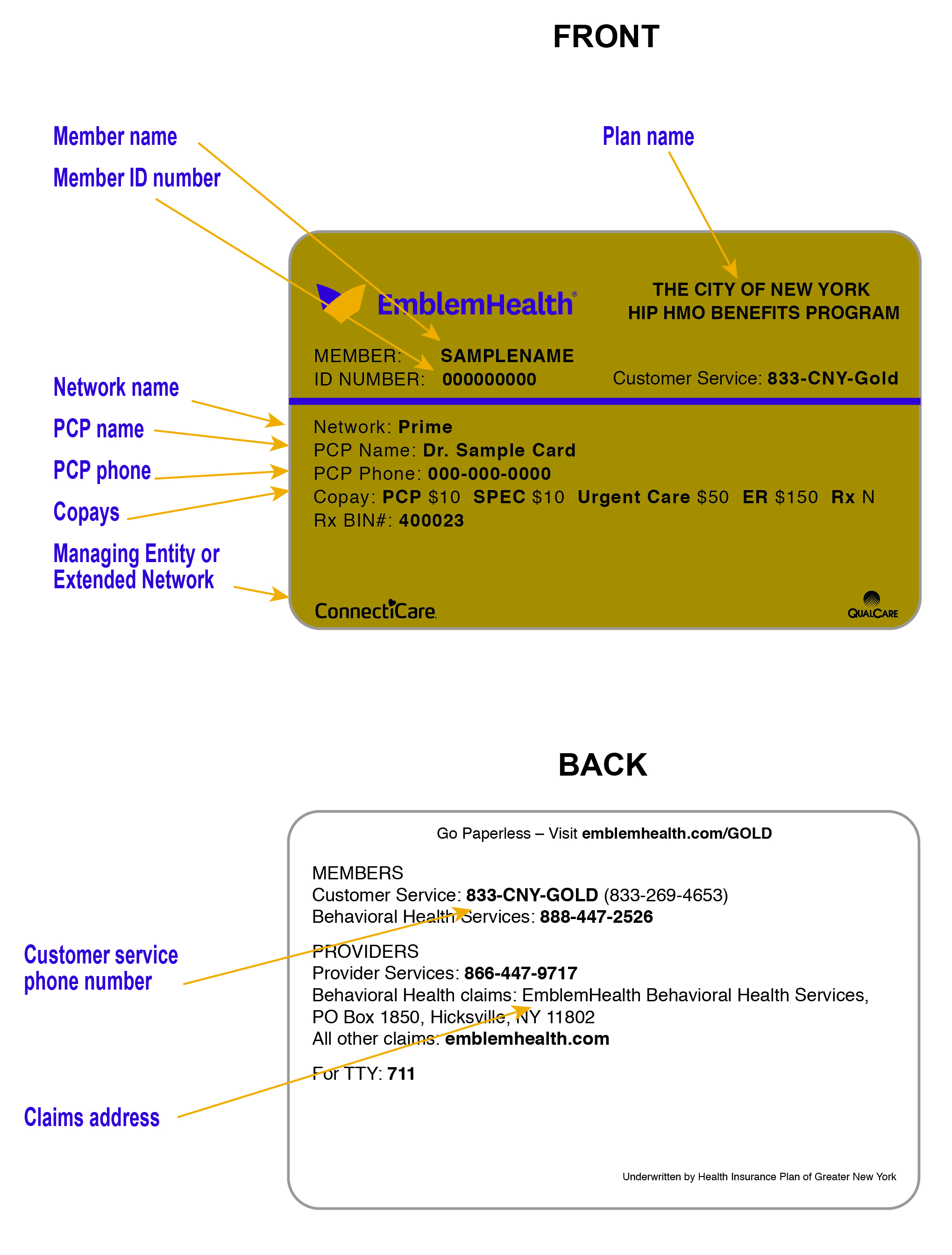
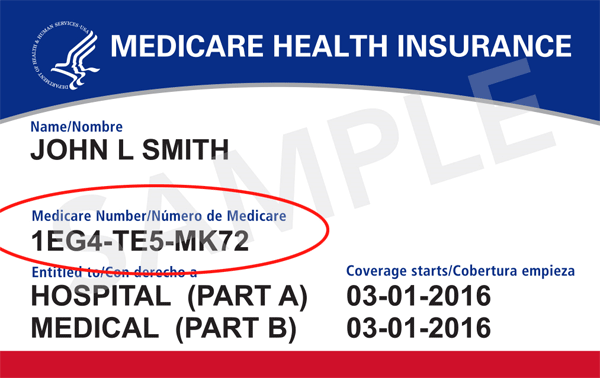
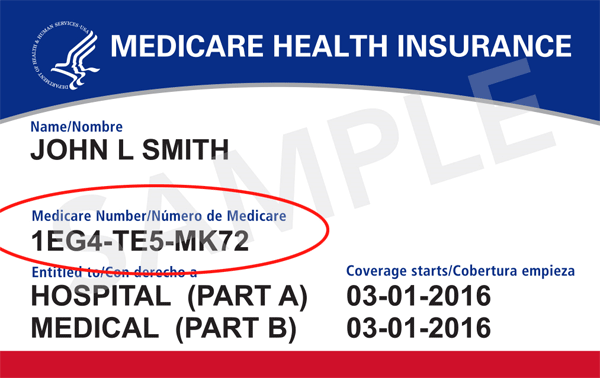
One plan becomes your primary plan, paying your claims first. The second plan becomes your secondary plan, which may pay toward the remaining cost, depending on the plan. Understanding which plan is your primary and which plan is your secondary is important to help prevent delays in claims processing. A member ID number and group number allow healthcare providers to verify your coverage and file insurance claims for health care services. It also helps UnitedHealthcare advocates answer questions about benefits and claims. You can continue to use the funds in your account tax-free for out-of-pocket health expenses.

If you enroll in Medicare, you can use your account to pay Medicare premiums, deductibles, copayments and coinsurance under any part of Medicare. If you have retiree health benefits through your former employer, you can also use your account to pay for your share of retiree medical insurance premiums. The one expense you cannot use your account for is to purchase a Medicare supplement insurance or "Medigap" policy. A qualified health-deductible health plan is a health plan with an annual deductible for an individual or a family that meet the minimum deductible amount published annually by the U.S. The annual out-of-pocket expenses required by the high-deductible health plan also does not exceed the out-of-pocket maximums published by the U.S.

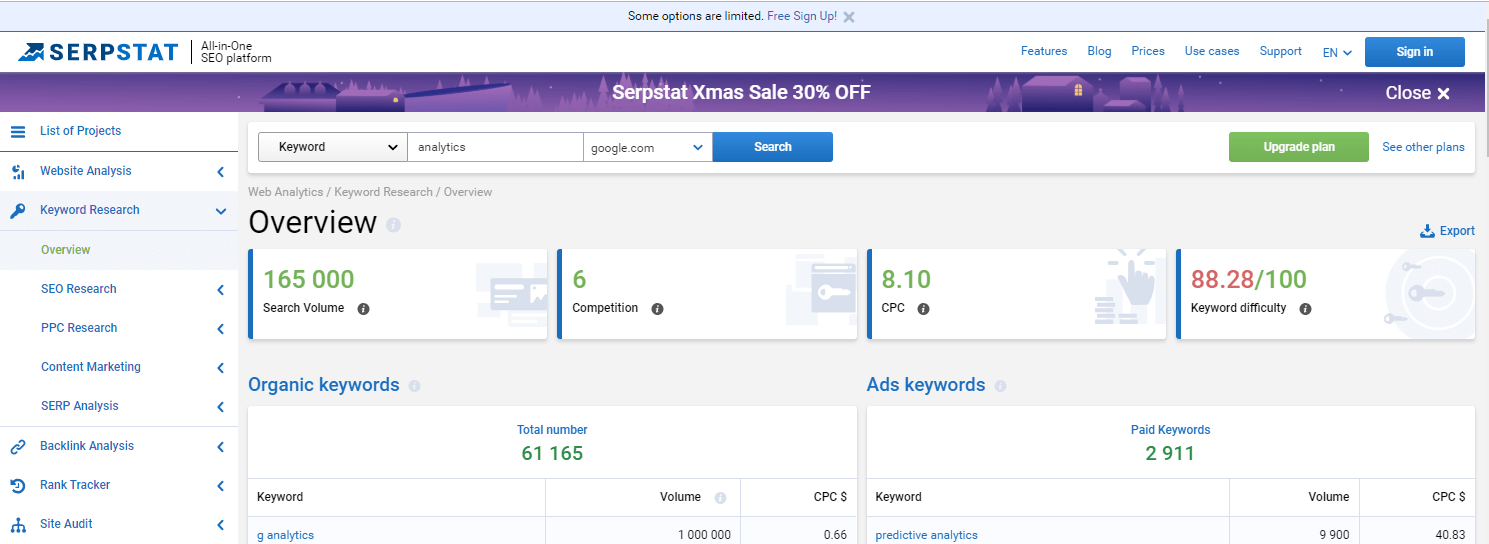
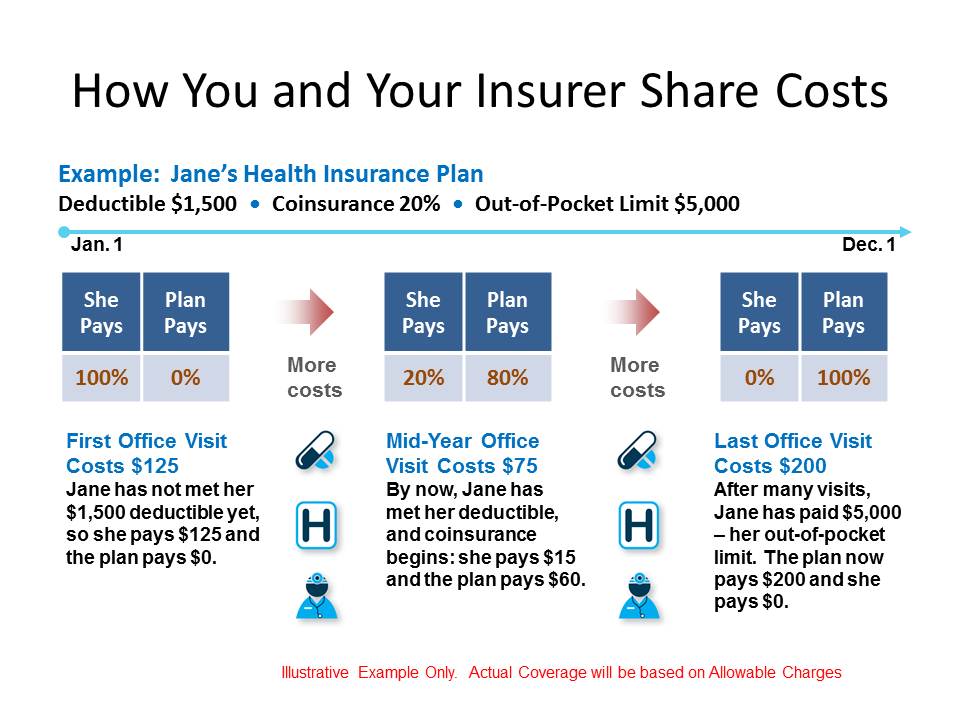
Out-of-pocket expenses include deductibles, copayments and other amounts the member must pay for, but do not include premiums or amounts incurred for non-covered benefits. Each payment you make for covered healthcare services you've received from your providers such as a physical exam counts toward your deductible. Once Blue KC processes the claims we receive from your providers showing the payments that you have made for covered healthcare services, we apply those payments toward your deductible. There are two times you can make a change to your enrollment options. Your employer schedules an open enrollment period once a calendar year when all employees may make changes to their health insurance plan. You may also make a change during a special enrollment period if you acquire a new dependent or if your coverage is terminated under another health insurance plan.

If you have health insurance through an employer, your group benefits administrator, typically someone in your Human Resources department, can help you make changes to your health insurance plan. If you do not have health insurance through an employer and instead pay your monthly premiums directly to Blue KC, call the Customer Service number listed on your member ID card. The back of your member ID card includes contact information for providers and pharmacists to submit claims. It also includes the member website and health plan phone number, where you can check benefits, view claims, find a doctor, ask questions and more. Your member ID number and group number allow healthcare providers to verify your coverage and file claims for health care services. These numbers also help UnitedHealthcare advocates answer questions about your benefits and claims.

EPO -- stands for Exclusive Provider Organization -- is similar to an in that it is a healthcare plan that covers eligible services from providers and facilities inside a network. Generally, an EPO does not pay for any services from out-of-network providers and facilities except in emergency or urgent care situations, which is similar to an HMO. Unlike an HMO, EPO participants are not usually required to have a primary care physician or referrals. After the funds in your PCA have been used, you will be responsible for a certain amount of your healthcare costs until your deductible amount has been met.
You do have the benefit of the negotiated prices for healthcare from network providers, but you will pay for all of the healthcare until your individual or family deductible is met. Distributions used for any other purpose are includable in income and may also be subject to an additional 20 percent tax. This 20-percent penalty tax does not apply to distributions made after your death, disability or attainment of age 65. Allowable charges are the maximum amount payable to you under your health insurance plan for a particular service. Contracted providers have agreed to accept this amount as payment in full.
For example, if the provider charges $100 for a service and Blue KC pays $80 as the allowable charge, the provider cannot ask the member to pay the remaining $20. Keep in mind, however, that some health insurance plans have coinsurance. In those cases, members are required to pay a percentage of the allowable charge. For specific details about your plan, review your Blue KC certificate, which outlines your payment responsibility. After you enroll in a private health plan and pay your first month's premium, you will receive a membership package with your insurance card and summary of benefits and coverage detailed information. A deductible is the amount that you are responsible for paying annually for healthcare services.

Exceptions are outlined in your Blue KC certificate, which lists the exclusions related to your health insurance plan. A copayment, or copay, is the dollar amount that you pay to a provider at the time you receive a service. For example, you might pay a $30 copay each time you visit your allergy doctor.

The copay amount is defined in your Blue KC certificate, which outlines your responsibilities for health insurance plan payments. A Primary Care Physician is the physician you choose to be your primary source for medical care. Your PCP coordinates all your medical care and knows your specific health history. You can designate a physician who specializes in family practice, general practice, internal medicine or pediatrics and is in your network as your PCP. Each dependent on your health insurance plan will also need a designed PCP.

Everyone on your health insurance plan may have a different PCP. Your children's coverage while they are away from home depends on the type of health insurance plan you have. If you have health insurance through your employer, check with your group benefits administrator for more information. Your PCP is listed on your ID card and in your online account. We recommend you call to make an appointment with your PCP as soon as you can. A checkup now will help your PCP learn about your medical history before any health issues occur.

Routine Preventive care is a care benefit that is not subject to a deductible. Your PersonalBlue health insurance plan includes a prescription drug coverage plan with set copayments for both generic and brand name prescription drugs. The PCA portion of your plan cannot be used to reimburse you for these copayments. Use your HSA debit card or other means provided by your HSA bank to pay for qualified medical expenses.

You should only use the debit card at healthcare-related locations. This may include an Internet transaction as long as the items being purchased are qualified medical expenses. You may also use your HSA debit card for online capabilities such as online bill pay. Billed charges are the amount charged or billed by your healthcare provider for the services/supplies you received. Not all provider charges will be paid by your health insurance plan.

If you have health insurance through your employer, check with your group benefits administrator to have a dependent added to your plan. He or she has the information and/or forms you need to add your dependent to your health insurance plan. Sometimes providers send statements to their patients before Blue KC has finished processing and paying the claim. If the provider you saw is out-of-network you will be responsible for paying the provider directly. We will send you a payment for the amount that is covered by your plan. You can view your EOBs and details about your claims, including how much you owe, by logging in and visiting the Claims and Usage section.

You might see a note on the bill that says "Insurance Pending." We will send you an Explanation of Benefits once we have processed your claim. If you are still unsure if you owe the provider, call their billing office. Please note, if your provider was not in the Blue KC HMO network, you will be responsible for paying all services and fees for seeing that provider.

Offering health insurance for individuals, families, employers and Medicare, our health plans give you coverage that's focused on your health and well-being. We are here to help answer your questions and find the plan that fits your needs. Facilities are defined as a general acute hospital, satellite emergency department or ambulatory surgical center licensed pursuant to the Health Care Facility Licensure Act. Effective Jan. 1, 2021, providers in Nebraska may not balance bill patients for medical care received from out-of-network providers or facilities in emergency situations.
This state mandate applies to all fully insured plans and non-ERISA groups. If a spouse has access to group insurance coverage through his/her employer, and chooses to decline that coverage to enroll in a Caterpillar healthcare plan, then the spousal surcharge will apply. Consequently, personal health insurance plans are not accepted.

Once your PCA funds are exhausted and the remainder of your deductible has been met, your health insurance plan will start paying. A majority of in-network expenses will be covered by your health insurance plan. Once your out-of-pocket maximum has been met, your health insurance plan pays 100% of your covered expenses. Yes, funds may be withdrawn and used to pay for qualified medical expenses for you and/or your tax dependent without a tax penalty. For purposes of medical deductible of a child of divorced or separated parents, they can be treated as a dependent of both parents.

Each parent can include the medical expenses he or she pays for the child, even if the other parent claims the child's dependency exemption. Please consult a legal or tax adviser concerning questions you may have. When you see an out-of-network provider, we send a check to you for the covered amount of those services. We will send you an EOB that explains how that amount was calculated. Yes, you must pay your copayment when you see your in-network provider. Your copayment amount depends on the health insurance plan you have and the services you are receiving from your provider.

BlueCard is a national program that enables Blue Cross and Blue Shield of Nebraska members to obtain in-network services while traveling or living in another state. The program links participating health care providers with Blue Plans across the country and internationally through a single electronic network for claims processing and reimbursement. Members can login to myNebraskaBlue to access cost estimates and cost comparisons for a variety of treatments and services. By logging in, your benefits will be applied to the estimate so you can see costs based on your benefit plan (copay, deductible, coinsurance, etc.). MyBlue offers online tools, resources and services for Blue Cross Blue Shield of Arizona Members, contracted brokers/consultants, healthcare professionals, and group benefit administrators.

24/7 online access to account transactions and other useful resources, help to ensure that your account information is available to you any time of the day or night. Your online account is a powerful tool for managing every aspect of your health insurance plan. Whether you need to check on a claim, pay a bill, or talk to a representative, you can easily access all your member features. You must use the BlueCross BlueShield of South Carolina card to receive medical or dental services, the Express Scripts card to fill prescriptions and the EyeMed card to receive vision care. Express Scripts is an independent company that contracts directly with the State Health Plan.

EyeMed is an independent company that contracts directly with the State Health Plan. Yes, but you will pay the full negotiated rate for ambulance and ER services until you meet your deductible, then you will pay co-insurance. For an ER visit, you also pay an extra $125 fee, which is waived if you are admitted as an inpatient. Non-emergency care should be treated at the physician office or urgent care facility to avoid the higher out-of-pocket costs. As a Blue Cross Blue Shield member, you and your covered dependents can receive treatment while traveling, including outside the United States.